In Part One of our two-part blog series on heart caths and donor management, we break down the key elements of an OPO cath lab report, starting with cardiac catheterization.
Ensuring comprehensive cardiac catheterization during donor management helps provide transplant surgeons with the detailed final report they need to quickly and confidently decide if a donor’s heart is right for their patient. With every minute counting, having access to clear data allows for faster decision-making, ultimately increasing the chances of saving a life.
“Transplant centers prefer to have a complete report, which includes the heart’s anatomy and pressure data and then summarizes the findings in the conclusions,” says renowned cardiologist and CompuMed chief medical director Dr. Robert Shiroff.
What is cardiac catheterization?
Cardiac catheterization is a procedure that involves inserting a catheter (a thin, flexible tube) into a blood vessel and guiding it toward the heart.
The process typically includes:
- Right heart catheterization: Measures pressures in the right atrium, right ventricle and pulmonary artery to give the most accurate representation of pulmonary circulation.
- Left heart catheterization: Evaluates left heart pressures.
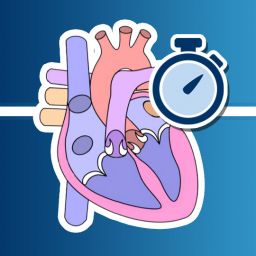
- Left ventricular angiography: Measures the heart’s ejection fraction, indicating if the heart is pumping adequately.
- Coronary arteriography: Provides images of the coronary arteries to check for blockages or other issues.
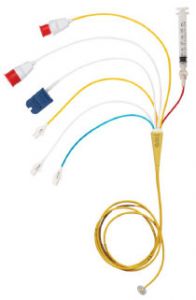

Dr. Shiroff notes that when performed in a cath lab with access to the proper equipment, each step of cardiac catheterization should only take a few extra minutes.
“For example, if you’re going in for the coronary arteriography and you’re entering the aorta, I believe you should go ahead and cross the aortic valve,” says Dr. Shiroff.
“Entering the vein is a separate step and may take more time, but I think the data to be gleaned from it is very important,” he continues.
What information should be gathered?
Completing the full procedure—if time allows—provides valuable insights that can aid in decision-making and improve organ viability for transplantation. These key measurements and imaging should include:
1. A minimum of two views of the right coronary artery, including the left anterior oblique (LAO) and right anterior oblique (RAO).
2. Multiple views of the left coronary artery, ensuring all major branches are clearly visible, including:
- The LAD (left anterior descending artery) and its smaller branches (diagonal and septal branches).
- The circumflex artery and its branches (called obtuse marginal branches).
3. Documented pressure measurements, such as RA, RV, PA and aortic pressure, as well as oxygen saturation and cardiac output, for right heart catheterization.
- Oxygen saturation levels are typically measured in the right atrium, pulmonary artery and aorta to assess oxygen flow to these areas and help detect the presence of any shunt lesions (abnormal pathway of blood flow) within the heart.
4. A specific angle called RAO (usually around 30 degrees) of the left ventricle, clear enough to estimate the heart’s pumping ability, known as ejection fraction (EF).
What is the significance of these elements?
These key measurements and images are critical for making the best transplant decisions.
For instance, when provided by your OPO as part of a request for a comprehensive donor heart evaluation, the reading cardiologist can provide the quickest and most detailed interpretation possible. Your OPO can then rest assured that a transplant surgeon will have everything they need to determine how well the donor heart is functioning.
“If you get these four things on a cardiac cath, any qualified cardiologist who does intervention or invasive cardiology can interpret these things and come up with a report,” says Dr. Shiroff. “The key then is to get the report to a transplant surgeon as soon as possible so that we can move forward with the transplant because we know timing is critical.”
What if I face resistance?
Dr. Shiroff acknowledges that while a transplant surgeon is looking for the information provided by cardiac catheterization, you may still come up against some initial reluctance from a cardiologist to perform the procedure on a potential donor.
He suggests referencing CompuMed guidelines for a comprehensive donor heart evaluation when facing any reluctance from clinical teams.
“A cardiologist might hesitate because it doesn’t have paid benefit to that patient, but it has benefit to the next patient, the intended transplant recipient,” says Dr. Shiroff.
“A cardiac catheterization is ordered because it’s needed to try and save an organ, and that saves a life,” he adds.
Ultimately, taking the extra steps to perform comprehensive cardiac catheterization isn’t just about collecting data; it’s about providing a complete cath lab report to maximize the chances of a successful transplant and give another patient a new chance at life.
Learn more about heart caths and donor management
In Part Two of our two-part blog series on heart caths and donor management, we’ll take a closer look at the significance of collecting and sharing cath lab pressure data, and how it can streamline your OPO’s workflow during donor evaluation and management.
For more of Dr. Shiroff’s insights, watch the on-demand episode of our Expert Webinar Series on Heart Cath and Donor Management, which includes an example of best practices for OPO cath lab reports.