Alisha Jackson, Senior Director of Organ Services, shares how ConnectLife’s partnership with CompuMed is redefining lung donor management and accelerating clinical decision-making to achieve a projected record number of lungs transplanted.
In this session, Alisha provides an inside look at CompuMed’s latest innovation — MOSAiCC™, an AI-augmented data capture and visualization platform built to transform organ recovery and transplantation.
Welcome everyone to another in a series of industry insights with CompuMed. It’s been a while as we’ve been focusing internally on developing, MOSAiCC. It’s our new data capture tool that we have the honor of Alisha Jackson going to share a bunch of updates from how her team has been using this. We’ve also been working with ConnectLife and CDTNY as kind of our beta partners, our development on this.
Some of you may have seen some of this at AOPO and since then we’ve had a lot more development. So just an administrative item. At the end of this we will have a Q&A. So in the chat or there’s a Q&A section sorry. You can drop your questions in and we will review those at the end. And you know for now let’s go ahead and hear from Alisha.
Alisha, thank you so much for joining us. We’re excited to hear about how you and the team at ConnectLife have not only improved processes, but, more excitingly, are on a pace for a record number of lungs transplanted in the year of 2025. So, Alisha, it’s all yours. Thank you. Thanks, Laura. As I said, my name is Alisha.
I’ve been with ConnectLife for about nine years. And we’ve been working with ConnectLife since 2016. We initially started with CompuMed as a sharing platform. So sharing of chest X-ray, CTs, as a quick way to be able to get those images to our transplant surgeons for quick viewing. In 2019, myself and a colleague went to CompuMed for echo training.
And we had implemented that due to the inability for serial Echos being able to evaluate heart consistent reads. And since implementation of our internal team completing Echos, we’ve had a huge increase in heart utilization. We recently just sent two more coordinators for training. It’s been an amazing program for our team. Working with the cardiologists CompuMed has been a great way for our team to learn, and also assist in donor management.
In 2024, we started engaging with CompuMed for the utilization of CT reads. So not only the image sharing, but also the reads. And then added in the 3D volumetric studies for abdominal organs and thoracic which has been huge in our surgeons being able to evaluate and make quicker decisions. March of 25. We started working on this MOSAiCC tool.
For assistance with lung utilization. We have a lung consultation specialist that helps with donor management. And we had needed a way to communicate that information to him. A little more clear. Without multiple text messages on multiple different platforms. So we started working with CompuMed to help build this tool, and it has been wonderful. As I’m sure most of the clinical teams and non-clinical teams know in here.
Good lung management is good donor management. So that really wanted to focus on our, growth in lungs. So just talking a little bit about our operational challenges, as many OPOs face. The clinical teams needed to move cases forward. Our had primarily been surrounding critical care nurses, respiratory therapists. We have administrators on call with critical care background as well as respiratory medical directors.
But we needed our clinical staff to not only be able to give us that information, but to also interpret it, make clinical decisions, and continue to move cases forward. And that’s a very specific skill set that can pose some challenges when it comes to hiring, training, onboarding. It can take a long time to have someone up and running.
In the OPO world, we all know we have very high turnover rate. We have high stress levels, long hours. We’re constantly facing staffing shortages, recruitments of critical care nurses and respiratory therapists can be difficult. And then not only that, but the training. It takes about 6 to 10 months for a coordinator to really become proficient, to be able to move cases forward.
Critically manage these patients, to successful outcomes. And that for all of us, I’m sure, in this OPO world know the financial burdens that that can take on, especially when when individuals don’t make it through orientation or becomes too difficult to continue. As I said, we have lots of different backgrounds. We have critical care nurses. We have respiratory therapists.
We have some nurses who have never worked critical care. And the donor management process is just challenging when you have to take all of these variables into account in order to make those decisions, to successfully stabilize the donor, to maximize lung opportunities. And the communication is not always the same. When I speak to a critical care nurse versus a respiratory therapist versus a non-clinical background, that communication is very different.
And some pieces, not by any fault of their own, get left out because of what that specific person is looking at. So our existing workflow didn’t support full data sharing. Not only with myself as AOC, but also with our lung specialist. A lot of what we were sending was text messages, quick clinical information. It was all pieced in part together.
And then his responses back were, also the same text messages, emails. A lot of what we had to do again was text messages. So you’re texting your entire ABG, you’re texting what the CT imaging was. We were having difficulty sending that information over. It was a lot of duplicate data entry and really delayed decisions for our AOCs as well as our pulmonologists.
To kind of give back to our team for donor management guidance. So with the development of MOSAiCC, and I’ll just speak a little bit about how it works. It can take information from many different platforms and many different ways to collect that data. So we have screenshots, static screenshots. If you can pull up a chest X-ray on your computer, you take a screenshot, upload that into the MOSAiCC.
You can also do screen recordings if you have a few pages of lab values. You can screen record and scroll through those lab values as quick as you can. There’s also opportunities for mobile uploads with your cell phone, so whether that be pictures of ventilators, pictures of bronchs, or the vitals or flow track, whatever you have, you can upload that with your mobile device.
The images taken on your mobile device are not stored there. They’re uploaded directly into the CompuMed platform. So there’s no need to worry about the HIPAA violation of having that information on your phone. We can also upload CDs. So your traditional CT scans where you have a CD, you can upload that. So all of those different modalities go into this MOSAiCC model.
And then what comes out of that is AI pulls all of the information that’s available through these different sharing techniques. We can also upload an XML file from our EMR platform. To pull information. So we’re not duplicate duplicating data entered there. And then AI can pull that information and create a very structured, summarized report. So what that does is it takes all of that information and places it into a report that we developed, along with our lung specialist, and how he wanted to look at things and how he wanted it presented.
What this did is it allowed us to then let him know we have the AI summary is up. He could take a look at that very quickly, put all of that information together and formulate a response. He was able to look at the CT scans, the images, if he wanted to look at more concrete data, not just the AI pool.
He could look at those images and be able to transfer that that information for donor management back to our team. So not only did it allow for quick upload. Our team is now down to about 10 to 15 minutes. They can get a full case uploaded into the CompuMed platform. And then the AI summary is available in about 5 to 10 minutes, and we can have that over to our lung specialist within an hour.
And have that information back to help direct our team for donor management and lung management. So, as I said, it takes all of this information that that you can obtain anything you can imagine. We’ve tried it with lots of different platforms. And all of that information comes into a very clear report for our specialists to take a look at.
And then, as I said, he then communicates back to us, for assistance with donor management. And then our team has a very clear cut path of what steps to take next. They can then re upload new imaging, new ventilator videos, new vitals, new flow track, new lab values. And AI summary is resythesized and our lung specialist can see where we’re at at that point.
So not only do we use this on potential lung cases, we actually started uploading every single donor. And so every donor gets uploaded. This is a great way for our AOCs to also have a very clear and clear cut information, on what’s going on with that patient.
We’re able to take a look at the AI summary. The spider graph has been something that I’ve really focused on. There’s a lot of modifiable factors to lung management but then also non modifiable. And so if we are on a side where we’re heavy with modifiable factors we know specifically we need to concentrate on lung management. And we can keep looking at that AI summary as we move through our cases to continue to evaluate our patients and see where we’re at.
One particular case, that we, we really use this for one of the first cases we uploaded the spider graph was very heavy in the not on the, in the modifiable factors. And so we took a look at this PF ratio. It was less than 150. We had done the lung management that we thought maybe was was helpful.
But because of this AI summary, we were able to look through and say, like, we’re not giving up. We had a dedicated employee that just went in for lung management. So that person was only focused on communication with our lung specialists, implementing the changes that he suggested, getting information back to him. And we were able to improve the lungs over a 24 hour time frame.
Which ended up leading to successful transplant. So that was one of our early cases that really focused on we need to continue to use this. We need to look at it. We need to make decisions based on it. And showed some successful outcomes. Our next case, which was just a few weeks after the initial case, was we had a 60 year old patient, which for us, as a small OPO, we had never had a six year old lung donor.
For a DCD the initial assessment, were not very favorable. But again, we looked at our AI summary. We were able to see there’s a lot of changes that we can make here. Prior to O.R., we had no acceptance and most of our centers were coding out for age in DCD. We felt that we had an opportunity here.
We did have tight time frames with this family. So, we called a known aggressive center, and they took a look at it. They took a look at our AI summary. They said they were willing to come. And that also ended up in a successful, successful outcomes. A slide that’s not in here is last week we had another patient that had less than favorable ratios.
We actually had exhausted the entire lung list. As we were doing lung management and working through, we kept updating the AI summary. I kept pulling it up and looking at it as the AOC. We actually ended up starting back at the top of the list again. We said we weren’t going to give up on these lungs.
I think some of the clinical coordinators think I’m crazy when I say start at the top, try again. But when we look at this, AI summary, it’s really hard as an AOC to not try again. And those lungs were also successfully transplanted. In just a few sequences down from starting that list all over again. So it’s just gives us concrete data to show our clinical team.
Look, we have an opportunity here and we need to not give up on this. The flip side, which our partners in developing this had also noticed is that, this was an ability to not necessarily have to focus on critical care nurses and respiratory therapists, but that we were able to shift our hiring, to still clinical roles.
But being able to utilize paramedics. This allowed for rapid onboarding. If somebody can utilize a computer and take pictures with their phone. They can get this information up into CompuMed and they don’t have to interpret respiratory acidosis or metabolic alkalosis. All they have to do is can they scan a picture to get it up into CompuMed, to pull into this AI summary, to go over to our lung specialist?
And then can they follow the step by step instructions from our lung specialists and implement those changes? So we have decided that we’re going to add every single case, to CompuMed and into this MOSAiCC platform because it does not only focus on lungs, but it gives us a really clear picture of what’s going on with that patient.
It reduces the variability from conversations. So I’m sure as AOC is, there’s a lot of individuals on this call who can say coordinator calls and says these lungs are no good. That doesn’t help us in making decisions. When you look at this, AI summary, it’s very clear you can look at the trends of the ABG is you can look at where they fall in the Salt protocol.
You can look at what are your modifiable factors. There’s no arguing any more with. Are you sure these are good lungs. Are you sure they’re not? It’s just very objective information and really removes a lot of the subjectivity of the coordinators based on their experiences.
So, so far this year, as of today, we have 18 lungs transplanted. Our goal for this year’s 20, when we created this PowerPoint, we were at 16. So we’ve just shown that this project really works well for us. As I said, we’re a small OPO. But 20 lungs in one year is a massive increase for us.
So we’re really excited to see how this tool can develop, how we can continue to work with CompuMed and in changing and developing this opportunity. So, as I said, the ability to make quick decisions so we can upload in about 15 minutes, 10 or 15 minutes, we can get everything uploaded that we need to get uploaded. We get an AI summary that we can take a look at as administrators, that we can take a look at either a medical director or a lung specialist.
There’s no details that are missed on it. We have everything we need to make the appropriate decisions. You can log on. You can share the AI summary the same way we share imaging. And, you can customize as an OPO what you’d like to specifically look at, what your workflows are, how you want your data presented.
And so there’s a lot of opportunity here for structure to tailor to what you need or what your subject matter experts need.
We are working on developing additional tools. There are advancements towards looking at heart and liver. So we’re working with compu med very closely in developing those two additional tools to really expedite and try to advance where we’re at.
Great. I will so Alisha, I, you know, I, I always, like I’m always a kind of the sap on this when you hear this when you’re working day to day. But the the number of lungs that you guys are going to end the year with is, just, just astonishing. Congratulations. Question I have, even though I talked to you quite a bit, what made you, especially like the case you had last week?
What made you keep pushing? Because I know you said at 4 a.m. you ran it again. You were just so confident that these were good lungs. So what? What compelled you to to just keep pushing that? I think it was having the AI summary right in front of me that was showing a F ratio that was trending up.
And then seeing on that that spider graph that there were a lot of modifiable factors still. So we can shift that focus and shift our management to trying to advance these lungs as best we can. And then we ended up with PF ratios in the four hundreds. And that’s when I told the clinical staff I was like, start over.
Like, we’re not giving up. We’re not giving up our PF ratios on initial assessment and initial allocation were I think, 250 to 300. So they were good, but we had just continued to improve and continue to work. They continued to speak to our lung consultation specialist doing donor management. And when they went up to the four hundreds and we had gone through an entire list.
There was no reason not to go back and start again. Another again. You know, I talk to you almost every week. As the whole team does. Not just myself. Sorry. I just happen to be the person on here for CompuMed. The other that we’ve learned a lot from, from you and also, you know, from, CDTN on theirs.
Is that the. You’re able to look at the data sooner, faster and been able to put the appropriate resources on it. Could you talk a little bit more to that? So, on that case that I spoke to that first case, we had taken a look at the AI summary and our ratios were very low. I want to say our starting was like 125.
And our patient was a full case. So very busy. When we looked at that AI summary within the first hour of the case, it made sense that we needed someone that could solely focus on lungs. Because of looking at this data, looking at where we were trending, our volume status on the patient, the flow track that we had up, it was very clear that we needed someone just focused on diuresing, recruitment that could communicate with our lung specialists directly and be able to just continue to focus.
So we made that decision pretty early on in the case because we knew we had tight time constraints from the family. And so we knew we didn’t have a lot of time to have our one coordinator be able to try to manage all of that. And so, like I said, within the first hour of the case, were able to make that decision to have someone just focus on lungs.
And speaking of the coordinators, how how easy has this been for them to to adopt and to learn and to incorporate it into your process? It’s been pretty easy. I think the first, training video that I made for them, I had never used the platform at all and just figured I would record my screen and see how it went.
And I think I get everything uploaded in like 10 or 15 minutes. Obviously I had seen what the platform looked like with the team. But once they started getting into it, there’s obviously a few technical things that they had to learn. And and some a few hiccups here and there learning how to use the technology.
But now our team can usually, as long as they have time, get everything up in there within about 20 minutes. From starting a case. And the other piece of that is we can have someone remotely in the background downloading a lot of the information, so we can have someone uploading information, getting it in there. And then really, all the onsite coordinator has to do is take a picture of the ventilator, take a picture of the monitor, video the bronch and get those uploaded whenever they’re available.
You you make it sound, so straightforward and easy. We’re glad to hear. Actually. Yes. Yes. It is pretty, but it’s been very easy for our team to learn. That’s that’s fantastic. One, one item that I wanted to I should have said at the beginning. So people wondered what MOSAiCC is. And I’m not going to test you, Alisha, because I actually, full disclosure, I had to text Lee to have him remind me what the, acronym is for, and it’s, it’s multimodal, synthesized AI, contextual capture.
So the tool has really we were calling it data capture at the beginning. And because really it is it’s about capturing data all in one place and then being able to use it.
So, Alisha, if there was any, you know, final, you know, lessons learned on it, what would be your biggest takeaway that you’re really excited about this?
I think what makes me most excited is we’ve shared and and all joking aside, that my feelings of of our donor management. So I’m not crazy telling people to start over again. It’s giving us very objective information. I think that the biggest piece that I take away is that now the data that I’m getting as an AOC making decisions, it’s no longer subjective.
I have a 2 or 3 page summary, gives me what the patient was admitted for, medical history, their trending of labs, their current bed settings, their fluid status, their their chest X-ray imaging, their CT imaging. I’m getting all of that information in one structured report. I don’t have to log on to the EMR in the middle of the night and try to find where was that CT scan, what did that look like?
So really the the objectivity and being able to make those decisions, right.
Thanks for joining us on another one of our Industry Insight webinars. Thanks, Alisha.
What You’ll Learn
- How MOSAiCC captures multimodal donor data (labs, imaging, ventilator settings, bronchs, vitals) in minutes
- How AI converts unstructured data into a structured summary, including PF trends and modifiable vs. non-modifiable factors
- Real case examples where MOSAiCC-supported donor management turned marginal lungs into successful transplants
- How MOSAiCC is allowing ConnectLife to move from a purely clinical hiring model (RNs and RTs) to more technical hires like paramedics — and how that’s driving efficiency.
Record-breaking results: How ConnectLife surpassed their 2024 lung transplant numbers by July, with MOSAiCC supporting a projected record year.
- How MOSAiCC’s intuitive dashboards are improving communication speed and quality between coordinators and clinical decision-makers.

Accelerating Improved Decisions by
Moving Data, Not People
About MOSAiCC
MOSAiCC by CompuMed is a secure, cloud-based platform designed to capture, visualize and share donor data – in context, in real-time. Built for organ procurement organizations, MOSAiCC streamlines donor management workflows and communication between coordinators, physicians and decision-makers — helping OPOs make faster, more informed decisions.

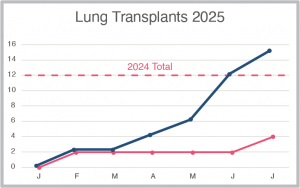 Record-breaking results: How ConnectLife surpassed their 2024 lung transplant numbers by July, with MOSAiCC supporting a projected record year.
Record-breaking results: How ConnectLife surpassed their 2024 lung transplant numbers by July, with MOSAiCC supporting a projected record year.